Written by Dhatri
Introduction
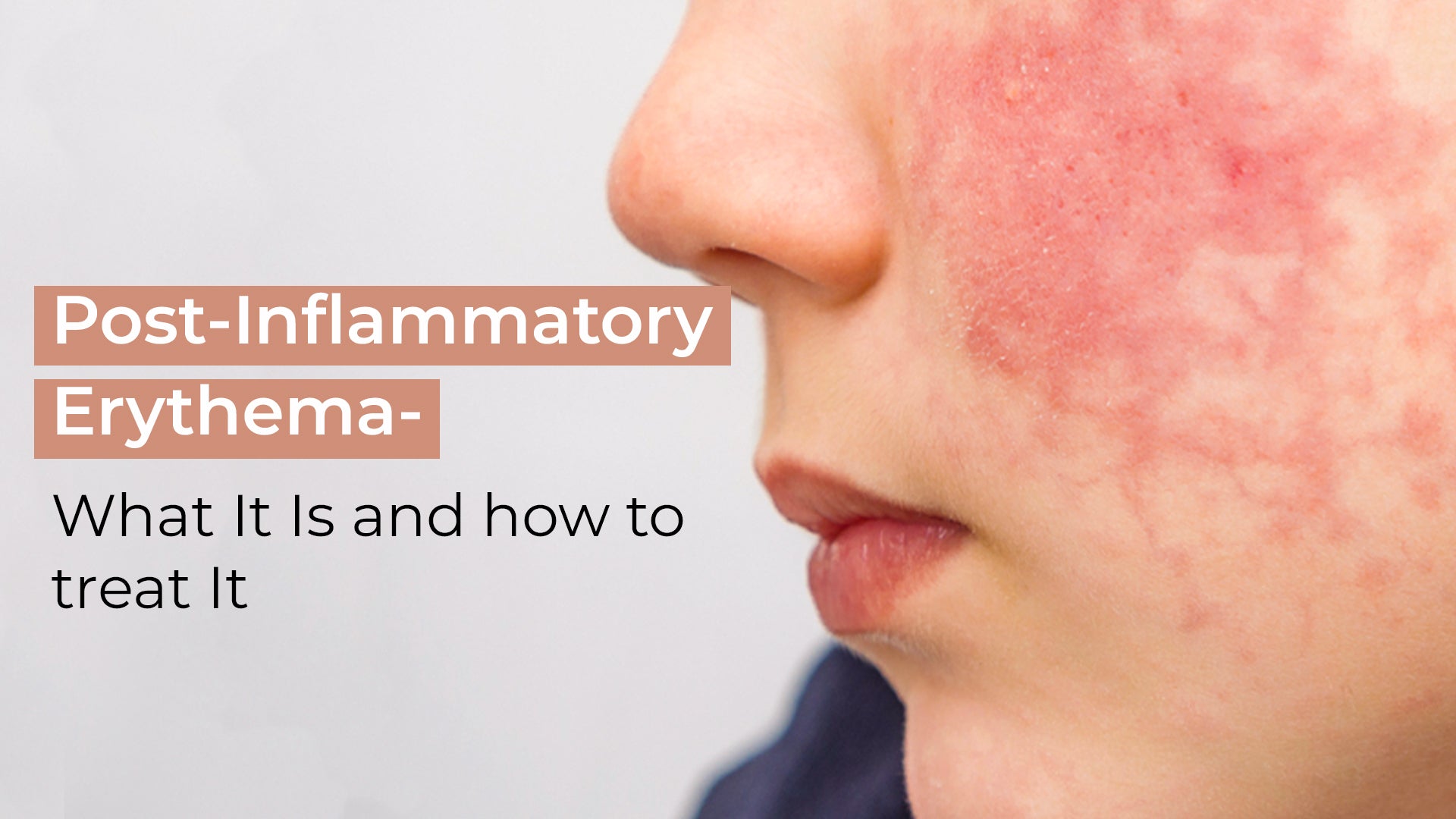
Did you face acne breakouts that leave marks on your skin of red, pink and purple marks on your skin? It is post-inflammatory erythema, which causes irritation to the skin and gives you a scarry look if you do not treat it well. So, you will understand in-depth what post-inflammatory erythema is? Additionally, how to treat it to give you a good look and prevent you from having skin problems.
What is post-inflammatory erythema?
Post-inflammatory erythema happens when blood flow stops during the inflammatory stage. Which leads to red or pink marks on the skin.
It does not occur only on the face; it causes it on the neck, chest, and back. Post-inflammatory erythema is more common in people with fair or dark skin.
Do you know the Causes of post-inflammatory erythema?
There are numerous causes of arising post-inflammatory erythema, the main reason is Cystic acne. It develops underneath your skin as a combination of bacteria, oil, and dry skin trapped under the pores. Although, cystic acne tends to occur in oily skin types.
Another reason is dilation, damage to blood vessels and inflammation as the skin has pink, red and purple marks. And using harsh products like soap, and scrub leads to redness and irritation on the skin because of post-inflammatory erythema.
How can you treat post-inflammatory erythema?
-
Niacinamide
Niacinamide consists of Vitamin B3, which reduces inflammation, keeps skin hydrated by controlling oil and strengthens the skin barrier. Additionally, it helps reduce the PIE and minimises cystic acne breakouts.
-
Vitamin C
Vitamin C is an antioxidant in nature that prevents erythema caused by ultraviolet B rays. It boosts collagen production and reduces redness in the skin.
-
Tretinoin
Tretinoin consists of vitamin A and is 10 to 100 times more effective than retinoids. It increases cellular turnover and chemically exfoliates the top layer of your skin, reduces inflammation and cleanses pores. Additionally, it repairs damages to the microvascular system and collagen that happen due to bacterial infection and reduces pH levels to normalise the skin. It is a prescription, so use it after consulting a doctor.
-
Sulfur
Sulfur consists of anti-bacterial, anti-inflammatory minerals, and keratolytic to prevent PIE and treat acne. Because it kills bacteria and sloughs away dead skin cells. It is famous for medical purposes.
Do not use it with exfoliates such as retinoids, benzoyl peroxide, and salicylic acid to dry and inflame your skin.
-
Aloe vera
Aloe vera is the ingredient that you might listen to for skincare and burn mark treatment. It contains vitamin A, C, E, saponins, amnionic acids, and anti-bacterial, anti-inflammatory, and hydrating ingredients. Which reduces the redness, irritation and inflammation experienced.
-
Clindamycin
It helps in killing bacterial causes of acne and reduces inflammatory breakouts by up to 50% within 12 weeks. This is slow compared to other treatments, but when clindamycin is combined with tretinoin, it boosts the treatment for post-inflammatory erythema.
-
Pimple Patches.
Are you a person who has the habit of picking or popping pimple patches? Because it helps in preventing inflammation and irritation of the skin, which reduces redness and scarring.
Bonus tips -
Never squeeze, touch, or scratch pimples or blemishes as this will aggravate them. Picking at pimples with your hands spreads bacteria, which causes breakouts.
References:
“Treatment of Acne with a Combination of Propolis, Tea Tree Oil, and Aloe Vera Compared to Erythromycin Cream: Two Double-Blind Investigations - PMC.” PubMed Central (PMC), www.ncbi.nlm.nih.gov, 1 Jan. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6298394/
“Flattening of Atrophic Acne Scars by Using Tretinoin by Iontophoresis - PubMed.” PubMed, pubmed.ncbi.nlm.nih.gov, 1 Jan. 2004, https://pubmed.ncbi.nlm.nih.gov/15075042/






 +91 9347578980
+91 9347578980